Car T cells therapy for autoimmune diseases
Chimeric Antigen Receptors (CAR) are receptors designed through genetic engineering techniques, with the aim of directing mainly T lymphocytes and NK cells to recognize and eliminate cells that express a specific antigen. CAR binding to target antigens present on the cell surface occurs independently of the major histocompatibility complex (MHC), resulting in robust T cell activation and powerful immune responses.
The four main components of CAR receptors are:
- Extracellular target antigen binding domain: Confers the specificity to bind to a specific antigen. To recognize a given antigen and induce T cell activation, the antigen-binding affinity of CARs must be high enough, but not high enough to cause activation-induced death of CAR-expressing T cells. and trigger toxicities.
- Hinge region: Provides flexibility and contributes length to allow the antigen-binding domain to access the target epitope.
- Transmembrane domain: Its most studied function is to anchor the CAR receptor to the T lymphocyte membrane. One or more intracellular signaling domains: The most common costimulatory domains are CD28 and 4-1BB (CD137); which are associated with high patient response rates.
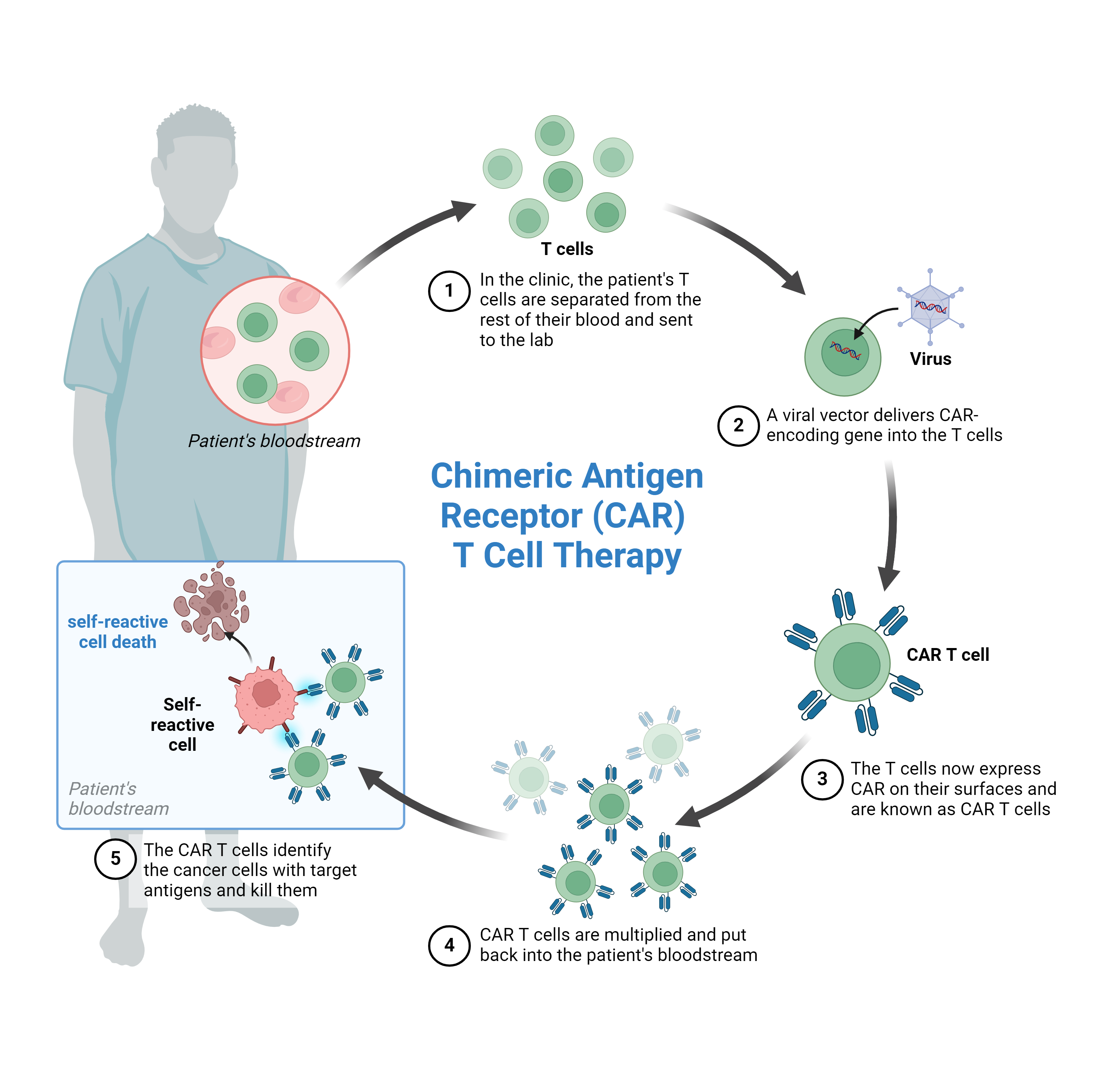
The manufacturing process of CAR-T cells begins with the isolation of peripheral mononuclear cells (PBMCs), using the Ficoll-Paque density gradient technique or by leukapheresis, then CD4+ and/or CD8+ T lymphocytes depending on the product. desired, enrichment and activation is performed, for which the cells are exposed to activating anti-CD3 and anti-CD28 antibodies attached to beads. To then carry out genetic modifications of the isolated T cells, using viral or non-viral approaches.
CAR-T cell manufacturing process, image extracted from Biorender.
Autoimmune disorders are a broad category of diseases with complex pathology. These disorders develop when the body's own immune cells (particularly autoreactive B and T cells) initiate abnormal attacks on their own tissues through a variety of effector pathways. These diseases arise from a combination of genetic predisposition and environmental factors.
To prevent autoreactive immune cells from attacking host organs, the treatment of autoimmune diseases remains to use broad, generally non-targeted immunosuppressive drugs, such as glucocorticoids and non-steroidal anti-inflammatory drugs, or their blockade with specific antibodies, such as antibodies against CD20 (Rituximab) or BAFF (Belimumab), antibodies against T cells, such as anti-CD52 (alemtuzumab), or against pro-inflammatory cytokines such as antibodies against TNF-α (infliximab). Autoimmune diseases can also be treated through hematopoietic cell transplantation, which can be autologous or allogeneic.
Cell therapy for autoimmune diseases has two approaches; eliminate and dampen self-reactive immune cells.
In a recent article published in The New England Journal of Medicine, researchers treated 8 patients with systemic lupus erythematosus, 3 patients with idiopathic inflammatory myositis, and 4 patients with systemic sclerosis; with a single dose of CD19 chimeric receptor (CAR) T cell infusion. All patients in the study had had a negative response to at least two previous immunosuppressive treatments.
Nine days after infusion, CAR T cells reached peak concentrations (146 per microliter), with CD19+ B cells being eliminated from the peripheral blood after 7 days.
After six months, patients with systemic lupus erythematosus presented remission, with the disease being absent for 29 months. In the three patients with idiopathic inflammatory myositis, after three months, creatine kinase levels and muscle function normalized; all patients discontinued corticosteroids and other immunosuppressive medications.
The data shown in this study provide new evidence of the short-term safety and efficacy of CD19 CAR-T cell therapy for autoimmune diseases, but clinical studies are necessary.
References
- Blache, U. et al. (2023) ‘CAR T cells for treating autoimmune diseases’, RMD Open, 9(4), pp. 1–9. Available at: https://doi.org/10.1136/rmdopen-2022-002907.
- De Marco, R.C., Monzo, H.J. and Ojala, P.M. (2023) ‘CAR T Cell Therapy: A Versatile Living Drug’, International Journal of Molecular Sciences, 24(7), pp. 1–22. Available at: https://doi.org/10.3390/ijms24076300.
- Müller, F. et al. (2024) ‘CD19 CAR T-Cell Therapy in Autoimmune Disease — A Case Series with Follow-up’, The New England Journal of Medicine, 390(8), pp. 687–700. Available at: https://doi.org/10.1056/NEJMoa2308917.